The intersection of artificial intelligence and medical science is currently fostering a new era of healthcare that was once the stuff of science fiction. For decades, the process of diagnosing complex diseases relied heavily on the trained eyes of radiologists and pathologists who manually scanned thousands of images for tiny anomalies. While human expertise is invaluable, it is also subject to fatigue, cognitive bias, and the sheer volume of data produced by modern medical facilities. Today, the integration of AI medical imaging is fundamentally changing this dynamic by providing a digital safety net that works with superhuman speed and consistency.
These advanced algorithms can detect patterns in pixels that are virtually invisible to the naked eye, allowing for the identification of life-threatening conditions like cancer or cardiovascular disease at their earliest, most treatable stages. This technological shift is not about replacing doctors but rather about augmenting their capabilities with powerful data-driven insights. As we continue to refine these neural networks, we are seeing a dramatic reduction in diagnostic errors and a significant improvement in patient outcomes globally. This guide will explore the technical mechanics of AI diagnostics, the various applications across medical specialties, and the profound impact this innovation is having on the future of clinical workflows.
The Mechanical Heart of Deep Learning in Medicine
To understand how AI “sees” a disease, we have to look at the underlying architecture of deep learning and neural networks. These systems are designed to mimic the hierarchical processing of the human brain.
A. Convolutional Neural Networks (CNNs)
CNNs are the gold standard for image recognition in healthcare. They break down a medical image into thousands of small features, analyzing edges, textures, and shapes to identify specific abnormalities like tumors or fractures.
B. Training Data and Pattern Recognition
An AI is only as good as the data it learns from. Developers feed millions of anonymized X-rays, MRIs, and CT scans into the system so it can learn the difference between healthy tissue and pathological markers.
C. The Role of Computational Power
Processing high-resolution medical images requires immense GPU power. Modern cloud computing allows hospitals to run these complex analyses in seconds, providing instant feedback to the attending physician.
Transforming Oncology Through Early Detection
Cancer remains one of the greatest challenges in medicine, and early detection is often the difference between a cure and a palliative care scenario. AI is proving to be a game-changer in this field.
A. Automated Mammography Screening
AI tools are now used to double-check breast cancer screenings. They highlight areas of concern for the radiologist, ensuring that small calcifications or masses are not overlooked during a busy shift.
B. Pulmonary Nodule Identification
In lung cancer screening, AI can track the growth of tiny nodules over time. By comparing historical scans with new ones, the software can predict whether a nodule is likely to become malignant.
C. Precision in Brain Tumor Segmentation
Identifying the exact boundaries of a brain tumor is critical for surgical planning. AI provides 3D mapping that helps surgeons remove the maximum amount of tumor while sparing healthy brain tissue.
Cardiovascular Health and AI Assessment
Heart disease is a leading cause of death worldwide, and AI is helping doctors identify risk factors long before a heart attack occurs. It brings a new level of quantification to cardiac imaging.
A. Automated Calcium Scoring
AI can quickly calculate the amount of calcium buildup in the coronary arteries from a CT scan. This score is a primary indicator of heart disease risk and allows for early lifestyle interventions.
B. Echocardiogram Interpretation
Reading a moving heart on an ultrasound is difficult. AI helps by automatically measuring the ejection fraction and heart wall thickness, providing objective data that reduces variability between different doctors.
C. Predictive Analytics for Stroke
In emergency rooms, AI scans brain CTs for signs of a stroke. By alerting the medical team within minutes, it ensures that life-saving clot-busting drugs are administered as quickly as possible.
Improving Radiology Workflow Efficiency
The modern radiologist is often overwhelmed by the sheer number of scans they must read daily. AI acts as a triage tool that helps prioritize the most urgent cases.
A. Smart Worklist Prioritization
Instead of reading scans in the order they were taken, AI flags images that contain “critical findings” like a collapsed lung or internal bleeding. These cases move to the top of the doctor’s list automatically.
B. Automated Reporting and Documentation
AI can generate preliminary drafts of medical reports by describing the findings it sees in the image. This allows radiologists to spend more time on complex diagnosis and less time on repetitive data entry.
C. Reducing Diagnostic Fatigue
By handling the “normal” scans that don’t show any issues, AI allows human doctors to focus their mental energy on the most difficult and ambiguous cases. This leads to higher accuracy across the board.
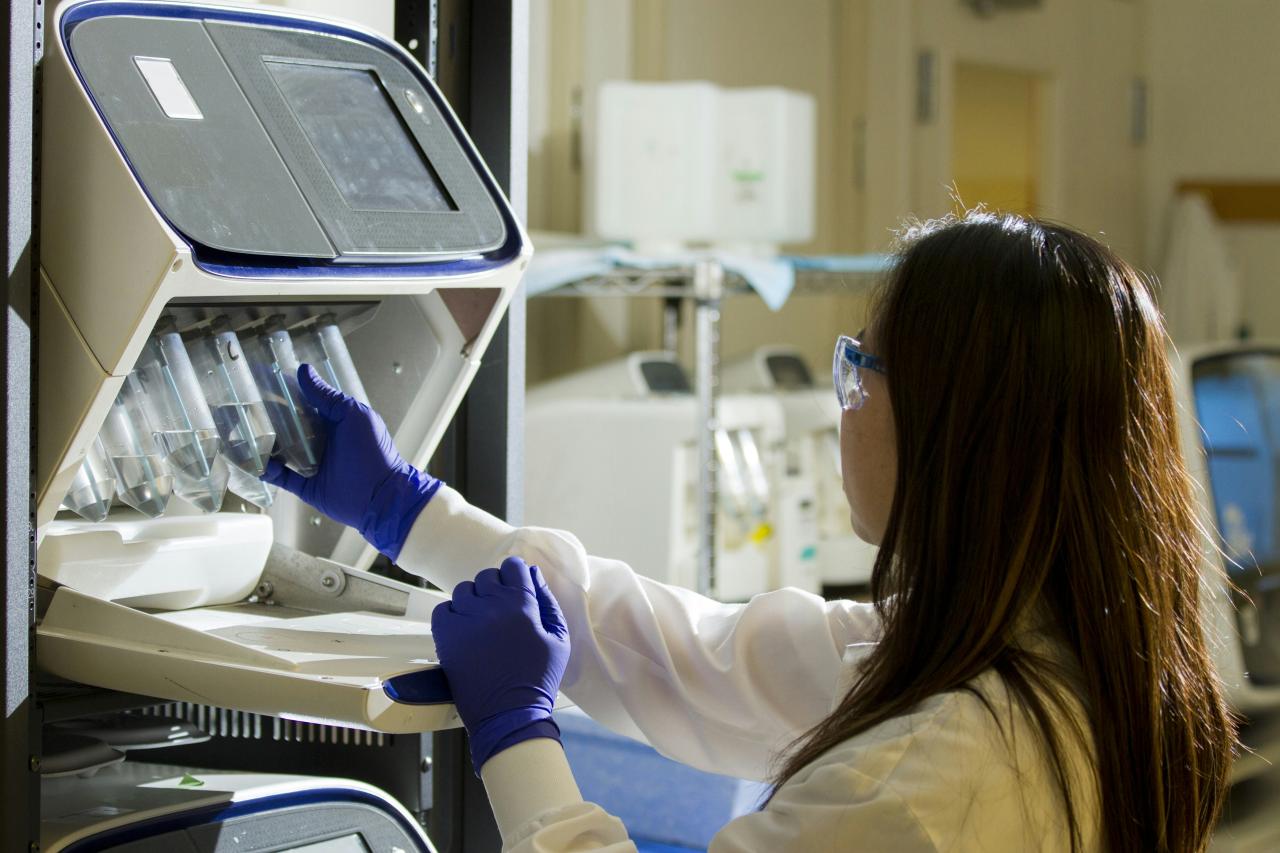
AI in Pathology and Tissue Analysis
Digital pathology is the latest frontier for AI, moving from the macro view of an MRI to the microscopic view of individual cells.
A. Whole Slide Imaging Analysis
Pathologists can now digitize glass slides and use AI to scan for cancerous cells across an entire tissue sample. This is much faster and more accurate than looking through a traditional microscope.
B. Biomarker Identification
AI can identify specific protein expressions in cells that indicate how a patient might respond to certain drugs. This is a core component of “personalized medicine” or “precision oncology.”
C. Predicting Genetic Mutations
Some AI models can predict genetic mutations just by looking at the visual patterns in a tissue sample. This saves time and money by reducing the need for expensive genetic sequencing in every case.
Expanding Access in Underserved Regions
One of the most profound impacts of AI medical imaging is its ability to bring high-quality diagnostics to areas with few specialist doctors.
A. Portable Diagnostic Devices
AI-powered handheld ultrasound devices allow nurses or general practitioners in rural areas to perform complex scans. The AI guides the user to get the right image and provides an instant preliminary diagnosis.
B. Telemedicine Integration
In regions without a local radiologist, AI can act as the first line of defense. It screens scans and only sends the most concerning ones to a remote specialist for a final check.
C. Automated Tuberculosis Screening
In many developing nations, AI is being used to scan chest X-rays for signs of TB. This allows for mass screening in high-risk populations where human doctors are in short supply.
Enhancing Patient Safety and Radiation Dose
Medical imaging often involves radiation, and AI is helping to make these procedures much safer for the patient.
A. Low-Dose CT Reconstruction
AI can take a “noisy” image from a low-radiation scan and clean it up to look like a high-dose scan. This allows doctors to get the information they need while exposing the patient to much less radiation.
B. Predictive Contrast Management
By analyzing a patient’s medical history, AI can suggest the minimum amount of contrast dye needed for a clear scan. This protects the patient’s kidneys from unnecessary chemical stress.
C. Reducing the Need for Repeat Scans
AI ensures that the first scan is done correctly by providing real-time feedback to the technician. This prevents the need for “re-takes” which would result in double the radiation exposure.
Challenges in AI Implementation
Despite its potential, the road to universal AI adoption in healthcare is filled with technical and ethical hurdles.
A. The “Black Box” Problem
It is often difficult for doctors to understand exactly why an AI made a certain diagnosis. Establishing “explainable AI” is essential for building trust between humans and machines.
B. Data Privacy and Security
Medical images are highly sensitive personal data. Ensuring that this data is protected from hackers while being used to train AI is a constant challenge for hospital IT departments.
C. Regulatory Approval and Standardization
Different AI models often produce different results. Regulators are still working on creating standard benchmarks to ensure that an AI tool is safe and effective before it can be used on real patients.
The Human-AI Partnership
The future of medicine is not about “Man vs. Machine” but rather about “Man with Machine.” This partnership is creating a new standard of care.
A. The Doctor as the Final Arbiter
AI provides the data, but the human doctor provides the context and the empathy. The final diagnostic decision always remains with the human professional.
B. Reducing Burnout for Medical Staff
By taking over the most tedious parts of the job, AI allows doctors to return to what they love: interacting with and caring for their patients.
C. Global Collaboration and Data Sharing
AI allows hospitals around the world to share “learned knowledge” without sharing private patient data. This collective intelligence accelerates the discovery of new diagnostic markers.
Future Horizons: Predictive Health
We are moving from a reactive “sick care” system to a proactive “health care” system where we find problems before symptoms even appear.
A. Multi-Modal Data Integration
Future AI will combine medical images with genetic data, lifestyle information, and real-time data from wearable devices. This creates a “digital twin” of the patient that can predict future health risks.
B. Real-Time Intraoperative Guidance
During surgery, AI will overlay diagnostic images onto the surgeon’s field of view using augmented reality. This will provide a “see-through” capability to avoid nerves and blood vessels during complex procedures.
C. Automated Longitudinal Tracking
AI will continuously monitor a patient’s imaging history over decades. It will detect the most subtle changes in bone density, organ size, or tissue texture that might signal the very beginning of a chronic condition.
Conclusion

AI medical imaging is fundamentally reshaping the landscape of modern clinical diagnostics. The technology acts as a powerful catalyst for improving the speed and accuracy of disease detection. Early identification of cancer and heart disease through AI is directly saving thousands of lives. Radiologists are benefiting from reduced workloads and a decrease in diagnostic errors. The integration of deep learning allows for the discovery of medical patterns invisible to humans.
Patient safety is enhanced through the significant reduction of necessary radiation doses. Healthcare in remote and underserved areas is becoming more accessible through portable AI tools. Pathology is moving toward a digital future where cellular analysis is both faster and more precise. The human element remains essential for providing the empathy and ethical oversight machines lack. Data security and privacy are paramount concerns that must be addressed as the technology scales.
Predictive analytics will soon allow us to treat diseases before they even manifest physical symptoms. The partnership between doctors and algorithms represents the highest level of modern medical care. Standardization and regulation are necessary to ensure the safety of all AI-driven diagnostic tools. As computational power grows, the possibilities for real-time surgical assistance will become reality. The ultimate goal of this innovation is a world where every patient receives a perfect diagnosis.